What size is that wound again anyway?
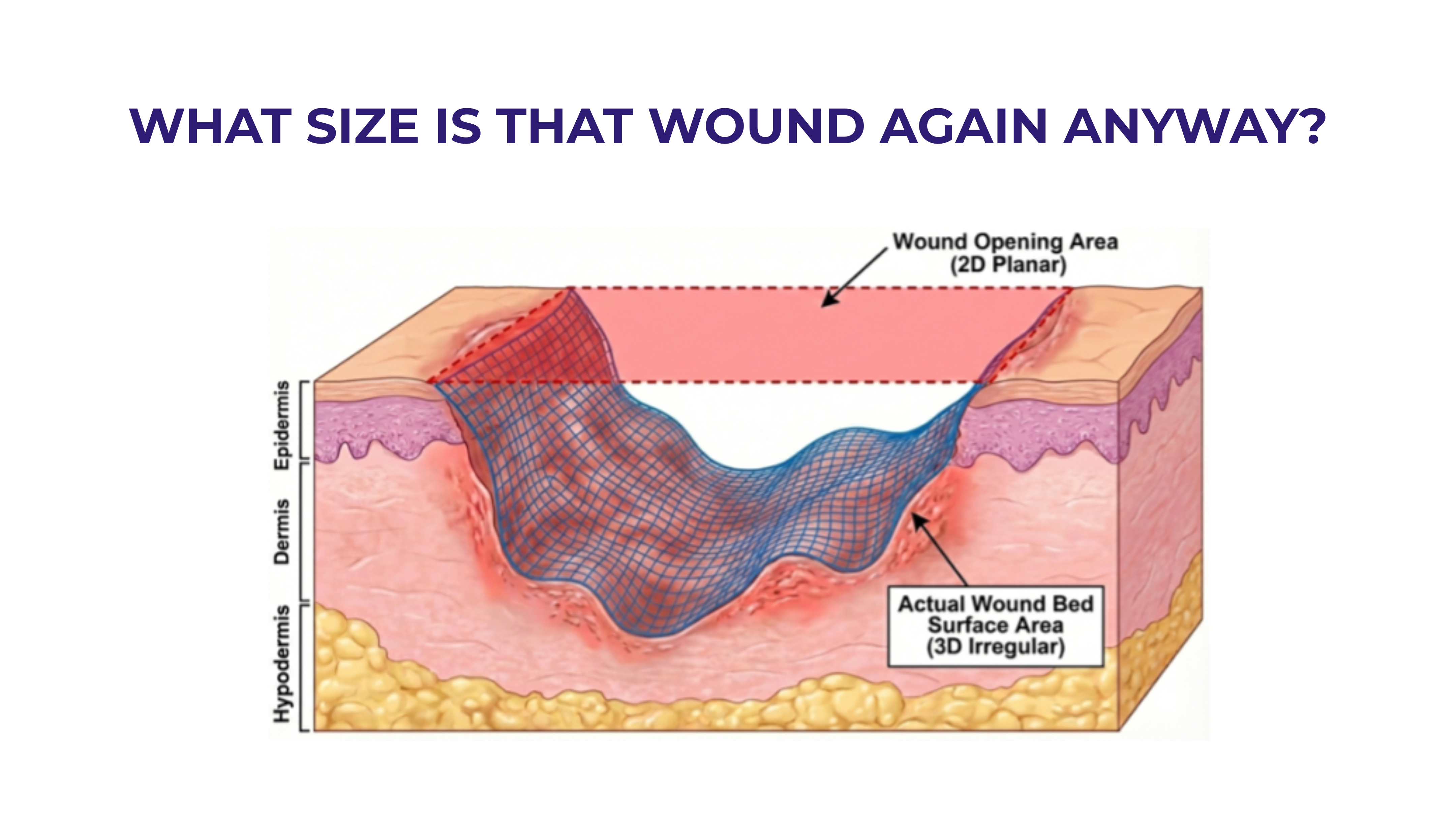
CMS's 2026 skin sub wastage policy allows providers to bill onlyfor units "administered," not "discarded." Cue the nightmare scenario: measuring grafts centimeter by centimeter to exactly fit the "wound area."
But here's the problem—what even is the wound area?
As several well-known clinicians have observed, there are two very different "areas" at play. One put it this way: “It’s a little like painting a room, do you want to just paint the ceiling or do you want to paint the walls too?”
In most wounds there is the 2D wound opening area at skin level—historically estimated as length × width, now calculable with modern AI tools. Then there is the actual 3D surface area of the wound bed. For skin substitutes to be administered as intended as a protective covering in compliance with FDA rules, it's the actual 3D surface that matters. That is what the graft contacts.
The gap between these two measurements is larger than most people realize.
Using simple geometric models: → Shallow wounds: up to 20% difference → Moderate depth: up to 100% → Deep wounds: 400% or even more
Calculating the true wound bed surface area requires full 3D surface mapping—not something you get from L × W × D. @ShaunCarpenter has proposed a clever drape-based estimation technique, but however you approach it, the wound bed surface you need to cover is likely substantially larger than the 2D opening suggests.
Now add to this the requirement for edge overlap. Many skin subs need to extend beyond wound margins to cover the wound edges and for fixation according to the manufacturer’s instructions for use. Even a conservative 0.5 cm overlap adds significantly—for smaller wounds, potentially an additional 100-200% of the wound opening area. For large wounds, it is still 25% or more.
So, what size skin sub actually needs to be "administered"?
The best available answer: highly variable, often substantially larger than L × W, and dependent on depth, geometry, and margin requirements that vary with every unique wound. This is way more complicated than adding up centimeter by centimeter to get some ideal “perfect fit.”
For now, the best measurement tool remains the clinician at the bedside—eyes, hands, and clinical judgment, carefully documented (with wound images) to explain why a particular size of graft was chosen.







.svg)



.jpeg)