The Crystal Ball: NO ONE HAS IT! A New Chapter in Wound Care From a Plastic Surgeons Perspective

My Story: I completed general surgery residency with a fellowship in wound care and Hyperbaric medicine. I went on to do an additional residency in Plastic Surgery, and once completed, I started my Plastic Surgery career with a continued interest and commitment to wound care.
The Turning Point
Just a few years ago, wound care looked stable. Physicians treated patients in clinics or hospital outpatient departments. Skin substitutes were valuable tools but not flashpoints. I personally was not a big proponent initially but continued to see the value, especially for non-surgeons and patients who were not good surgical candidates. Then came 2020—and everything changed.
When COVID-19 swept through, clinics closed, and hospitals locked down. Chronic wound patients, the ones least able to wait—suddenly had nowhere to go. Providers saw it firsthand: diabetic ulcers worsening, infection rates climbing, amputations rising. Out of necessity, they adapted. Patients requested alternatives to coming into the offices to receive care. Telemedicine, then taking care directly to patients—into nursing homes, and into homes themselves. The mobile wound care model wasn’t born out of ambition—it was born out of compassion. But this was not a new invention. Many providers “dabbled “in the mobile space because it seemed logical that patients with mobility issues would benefit. But now with more technology and demand, the mobile model has gained momentum, and clinicians and patients have seen the benefits.
In the meantime, advanced therapies were also evolving. The ability to achieve healing in patients who were not surgical candidates, by using advanced tissues and matrices excelled. Skin substitutes, now termed (CAMPS Cellular, Acellular Matrix Products), which encompasses the vast majority of the advanced tissue forms allowed for wound healing and progression in patients who otherwise were struggling to heal. As the demand increased, the policies and procedures around their use started to change.
The Policy Shift That Changed Everything
While providers were reinventing care based on patient needs, CMS’s Average Sales Price (ASP) reimbursement model for skin substitutes (CAMPS) was breaking down.
ASP was meant to control prices by tying reimbursement to the average sales price, factoring in manufacturer discounts. In some contexts, that approach works. But in wound care—where entry barriers are low and list prices are unconstrained—it had unintended consequences.
New products flooded the market. Prices rose. Reimbursement followed. The result: a booming, but unsustainable, ecosystem where the most entrepreneurial providers could make a living seeing just a handful of patients a day.
The Candle Wax Begins to Melt
For a time, it seemed like a golden era. Mobile services provide a light to the dark tunnel of wound gloom. The providers included physicians and nurse practitioners who enjoy their autonomy away from larger less flexible hospital systems, and patients enjoyed receiving personalized advanced care in their home or living space. The system appeared to work and at first it did. However, the scales were not balanced. And quickly the imbalance resulted in chaos. Incentives were misaligned, spending ballooned, and efficiency lagged.
So here we are with the 2026 Physician Fee Schedule set to make a 90% reduction in reimbursement. The wax that held this model together and gave light and hope for patients and providers is melting fast. Providers who once needed to see four or five patients a day may soon need to see many more to stay afloat, and this most certainly will diminish the quality and personalized care delivered.
Some providers will not be able to continue. The available providers will dwindle. Small mobile practices may be absorbed by larger systems or exit altogether. Some locales may be left with few if any provider options. While the demand for patient care will continue to rise, there will be limited resources to accommodate.
The Cost of Fragmentation
Already, hospitals and ACOs are sounding alarms about overspending and fragmented care. The journey from hospital discharge to healing remains dangerously inconsistent: a patient leaves the hospital, fails to see a specialist, misses follow-ups, develops an infection, and returns to the ER.
CMS has fortified their commitment to reevaluate ASP Methodology for Skin Substitutes to ensure reimbursement reflects both clinical value and fiscal sustainability. Thus far, controlling costs has been accomplished only indirectly through what many would characterize as audit weaponization. While this tactic gives way to more permanent and appropriate solutions, there will be opportunities for providers and practices to close gaps in aligning patient and financial outcomes. Each gap adds delays. With each delay, there is an additional risk. And every missed opportunity brings us closer to an amputation or wound septic event leading to death which could have been prevented. The care facilities will immediately return patients for readmission and/or recommend additional ER visits, both of which are costly to the patient and the health care system. This isn’t just a reimbursement issue; it’s a patient’s safety issue, and a global concern for continued health care.
Now what? We need a Vision for Integrated, Accountable Care
The next chapter of wound care must be written around integration, coordination, and accountability. Imagine: a patient’s care begins in the ER, primary care clinic, or hospital. A multidisciplinary team—vascular, podiatry, nutrition, wound care—assembles around them in a hub-and-spoke model. The patient stays in one place while the specialists rotate. Once the plan is set, mobile wound care teams carry it out in the patient’s home or nursing facility. They are an integral part of the health care team.
Hospitals, home health agencies, and specialists all share the same goal: healing the wound before it becomes catastrophic.
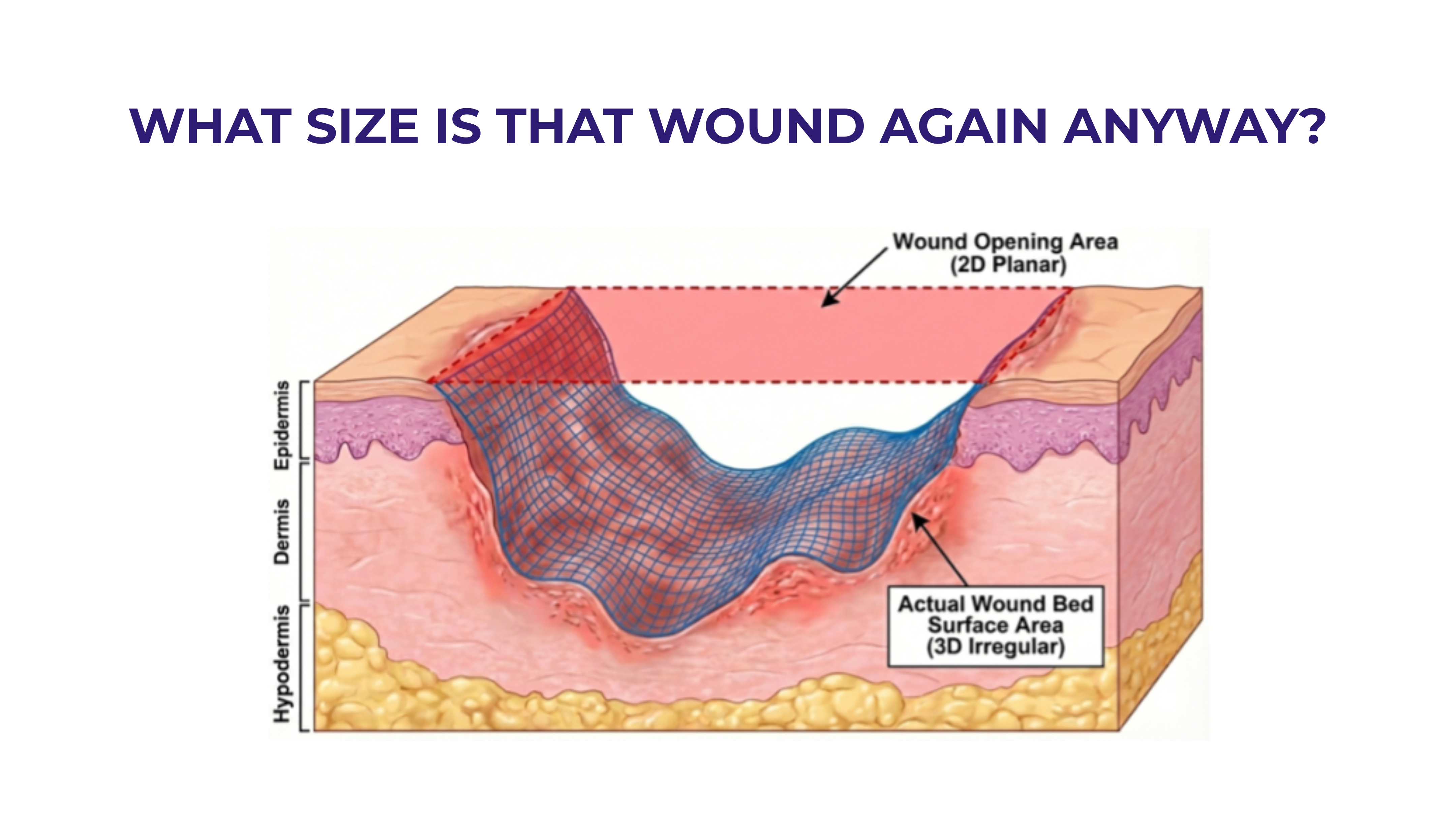
This is not a distant vision; it’s a practical necessity. Studies show that if a wound isn’t at least 50% healed within four weeks, the odds of full healing fall to just 10–11% per month thereafter. Time is tissue. Speed matters. Coordination of care saves lives. An integrated approach is needed.
Hub-and-spoke systems that connect hospitals, specialists, and mobile teams will become a reality. Analogous models are cancer care centers. Placing the patient first and at the center of the flow will positively impact their care and the ease with which it is delivered.
How practices fit into this will vary; some may decide they can evolve into more sophisticated vertical organizations that can market their results, both clinical and health economically to fuel their organic growth; others may decide their best place is as a part of a large collaborative practice; and still others may exit and look for opportunities that fit their preferences more closely. Those who stay and grow will need to support innovation and data transparency in wound healing outcomes. The patients will dictate the model, and it is the responsibility of the providers to recognize the vertical need for continuity of care such that each level of care is addressed.
This may include:
• Use of shared electronic wound registries to track progress and outcomes.
• Promoting technology-enabled coordination between hospitals, home health, and mobile providers.
Looking Ahead---Completing the picture
The story of wound care has been one of adaptation, and that story is still evolving. The next phase will be no different—but this time, we have a chance to design the system intentionally.
If we align incentives with outcomes, empower collaboration, and restore sustainability, we can ensure that the next chapter in wound care is simply better. —both for patients and for the healthcare system itself.
The future isn’t uncertain. It’s unwritten—and now is the moment to pick up the pen



.svg)



.jpeg)