The price patients will pay for the PFS

After a recent survey we conducted, it is clear most clinicians agreed skin substitutes are highly effective and essential, warning that the proposed rates would reduce patient access, hinder innovation, and threaten the viability of many practices. Read the blog to learn more about our findings.
The entire wound care community has expressed serious concern about CMS’s proposed changes to skin substitute coverage and reimbursement, including the proposed 2025 Physician Fee Schedule (PFS). To gauge the response of clinicians to CMS’ proposals, we recently conducted a survey of mobile and office based wound care specialists. Additional surveys are in process to gather more information about this critically important subject.
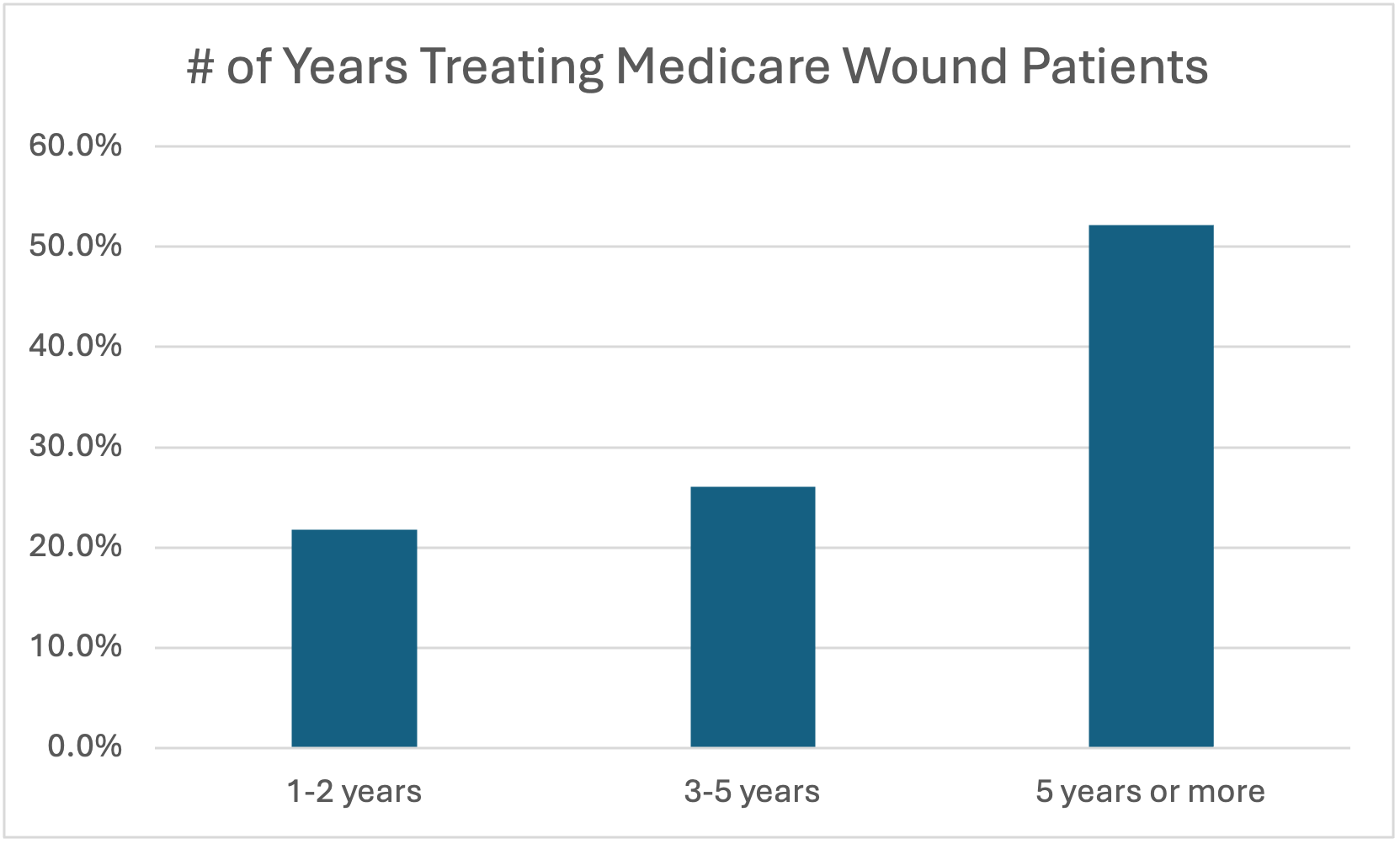
Of the clinicians responded to our survey, the large majority had multiple years of experience treating Medicare patients with chronic wounds.
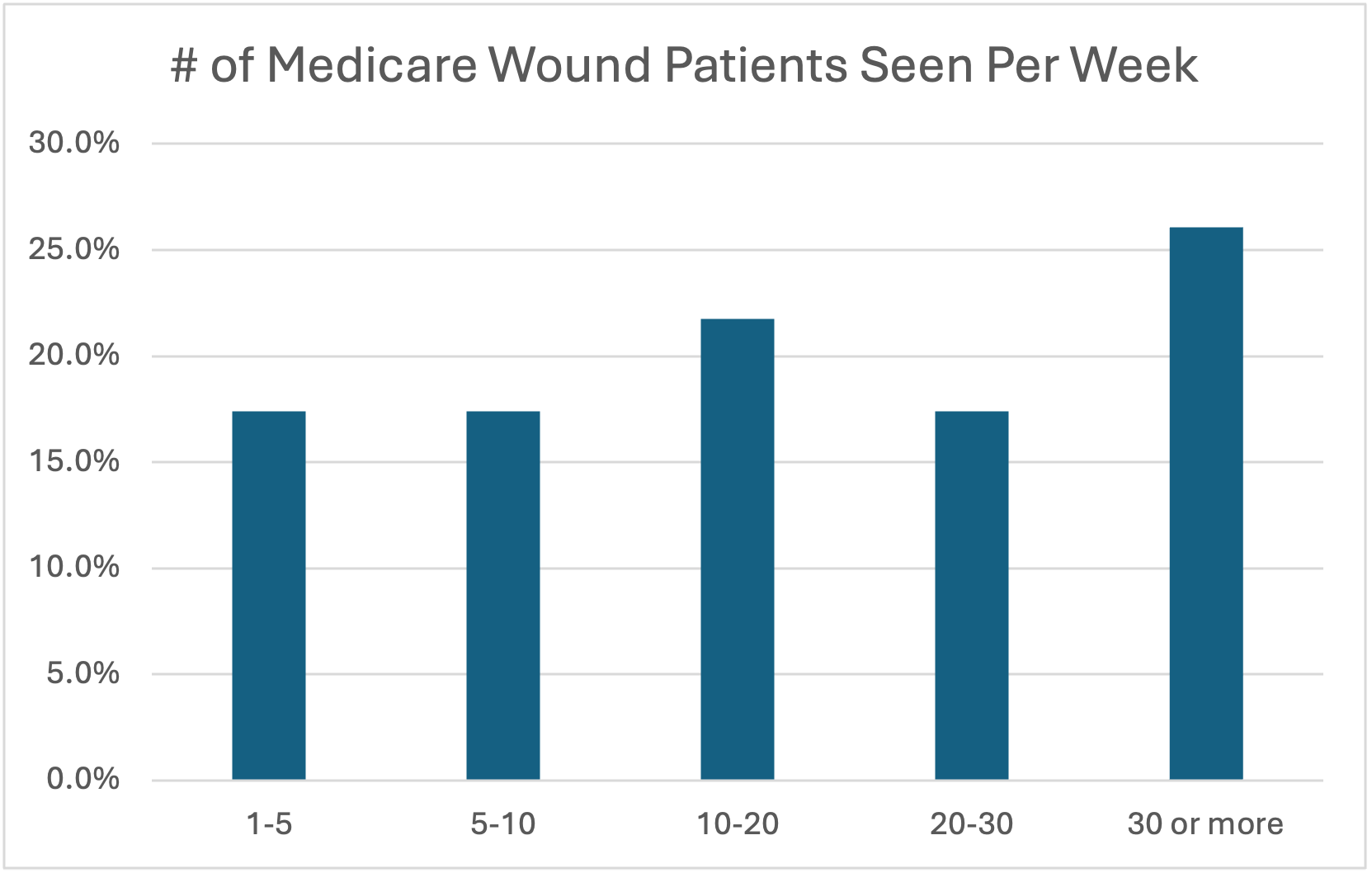
Likewise, the majority of responding clinicians were seeing 10 or more Medicare wound care patients each week, with more than 25% of clinicians seeing 30 patients or more on average.
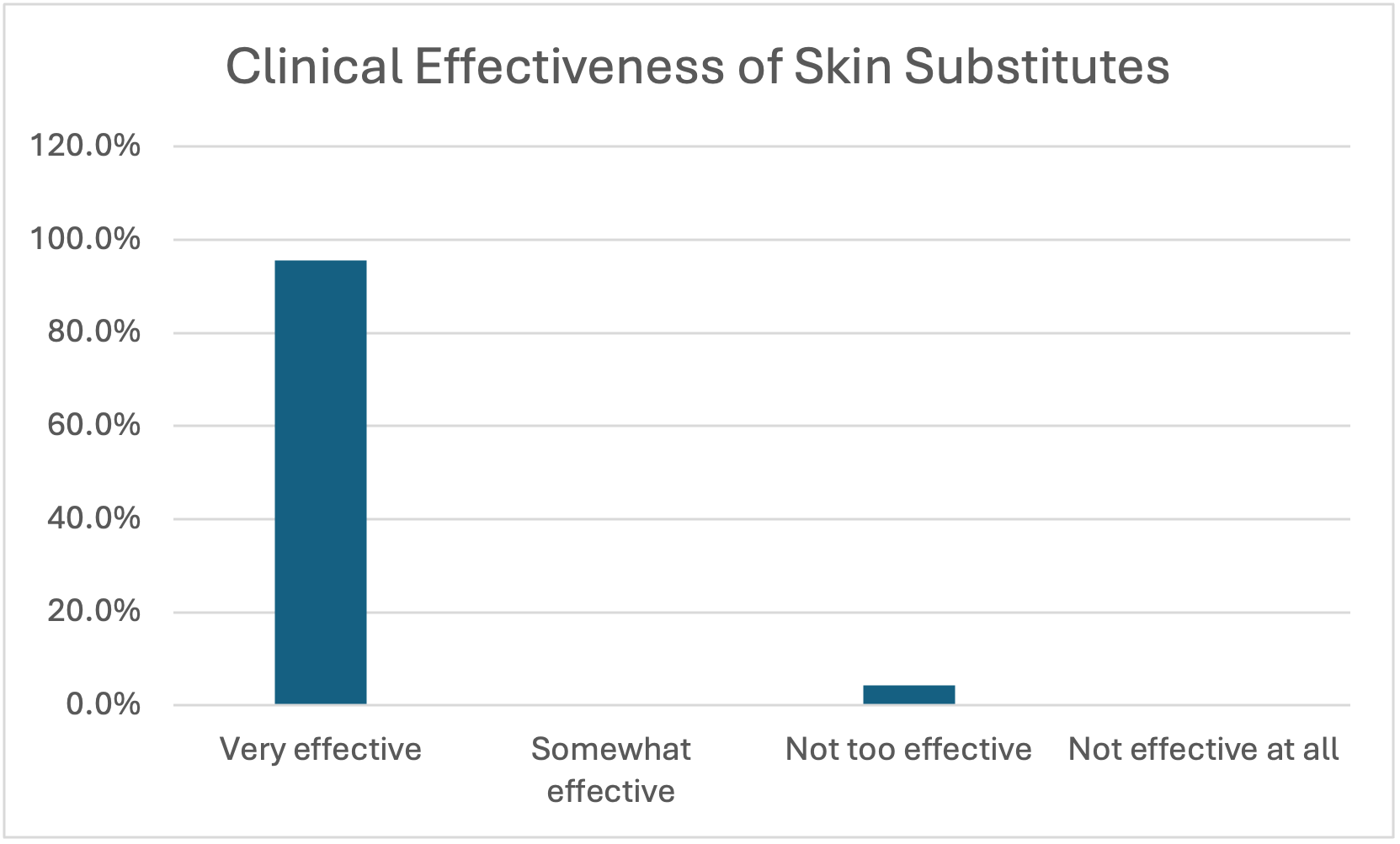
The responding clinicians were virtually unanimous in their opinion that skin substitutes were “very effective” in the treatment of their patients.
The vast majority also viewed skin substitutes as very important to the clinical treatment of their wound patients.
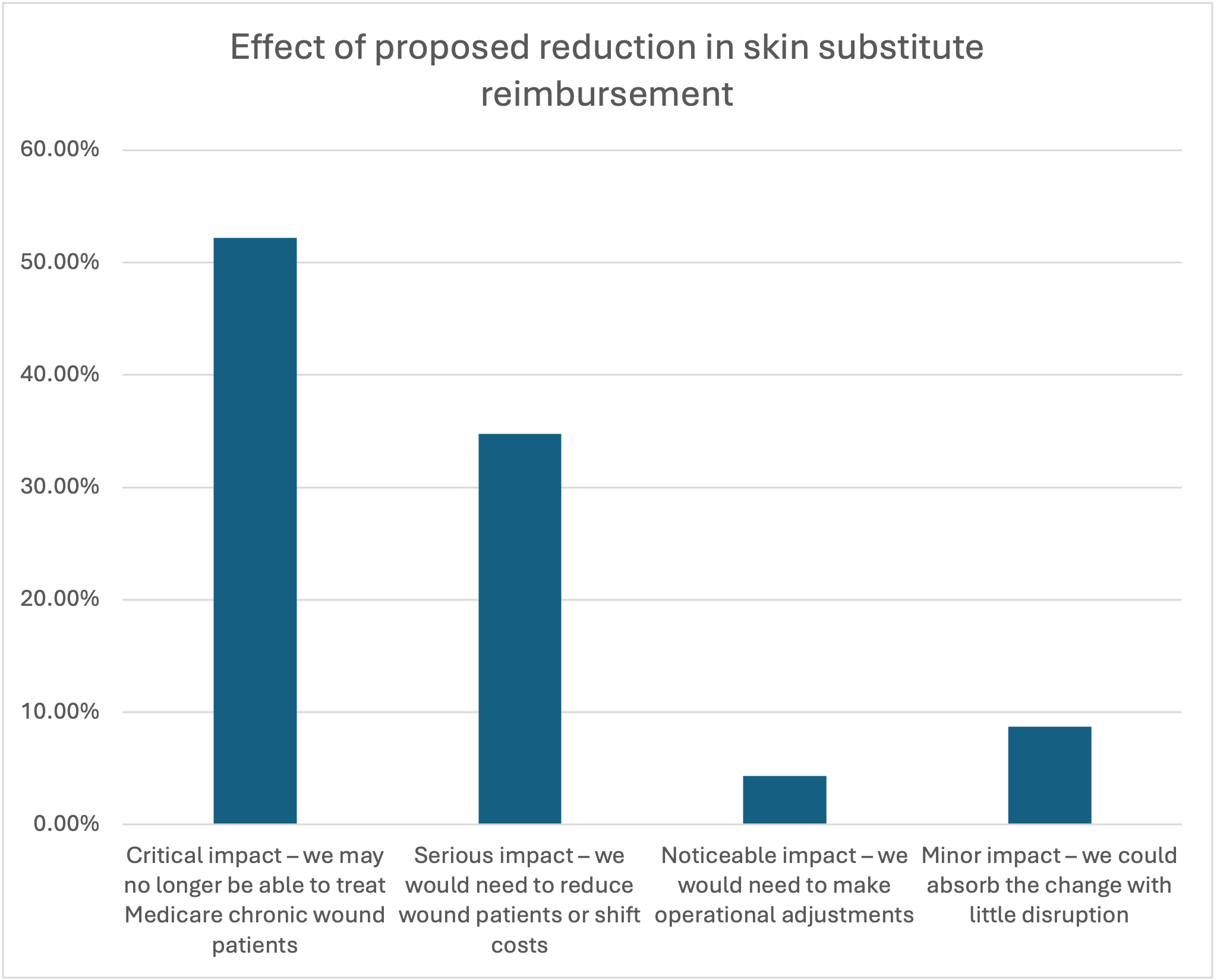
These clinicians as a group were very concerned about the impacts of the proposed skin substitute reimbursement reductions, with 87% reporting that the proposed changes would have either a “critical impact” or a “serious impact” on their practices and their ability to treat Medicare wound patients.
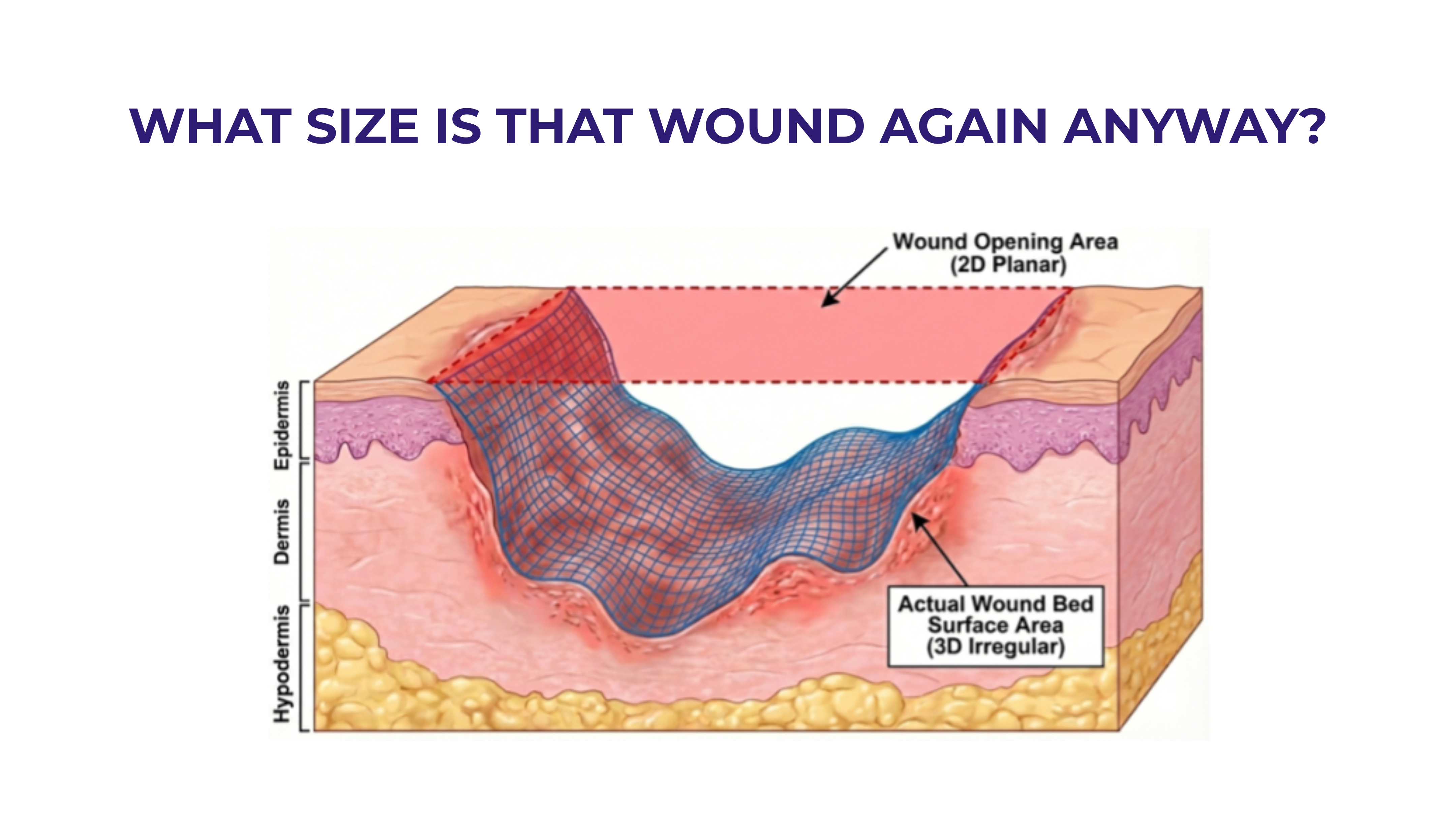
When asked about specific possible reimbursement rates, more than 60% responded that at a reimbursement rate of $500 per sq centimeter or below, they would be forced to start reducing their use of skin substitutes for Medicare patients due to financial constraints. Many also responded that they could be forced to change their practice and stop seeing chronic wound patients in their current business model altogether. This would obviously lead to negative long-term impacts on patients, but there are even more challenges anticipated should the currently proposed $125.38 price become effective.
There is also the problem with low application code reimbursement pressuring the manufacturers to discount in an unsustainable manner. Specific to application fees, the proposed PFS professes to achieve reimbursement parity among providers in all places of service but fails to address that the physician portion of the application code in the HOPD place of service is now and will remain about $780.00 but is only about $150 in the private office and mobile settings. The implications of this disparity are that independent physicians will remain in a position where they could be forced to choose the lowest priced product available regardless of scientific or clinical evidence, and as a consequence, innovation would disappear from the market. Longer term, the producers will disappear, leaving the lowest priced and likely the least effective products in an oligopoly which will again lead to price escalation problems. Raising the physician application fee to parity with the HOPD would significantly mitigate this issue. More than 80% of survey respondents indicated the current physician fee for skin substitute application is too low and should be raised.
Wound care is a challenging field of practice with limited reimbursement and growing numbers of patients requiring treatment. Reductions in the availability of treatments and providers would seriously impact patient access. CMS should carefully consider the collateral damage its proposed policies might cause before settling on an appropriate set of reimbursement rates.







.svg)



.jpeg)