Venture Medical's Official Comment On The Physician Fee Schedule
We have asked our industry to make their voices heard and submit their comments to their local and federal legislators regarding the 2026 Proposed Fee Schedule. In this blog post we share our official comment.
September 12, 2025
VIA ELECTRONIC SUBMISSION
The Honorable Mehmet Oz, M.D. Administrator
Centers for Medicare & Medicaid Services
United States Department of Health and Human Services Attention: CMS-1832-P
P.O. Box 8010
Baltimore, MD 21244-1850
Re: Comment on Medicare and Medicaid Programs: Calendar Year 2026 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; and Medicare Prescription Drug Inflation Rebate Program – File Code CMS-1832-P
To Dr. Mehmet Oz:
Venture Medical, LLC (“Venture” or “Company”) appreciates the opportunity to provide comments regarding the Centers for Medicare & Medicaid Services’ (CMS) Calendar Year 2026 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; and
Medicare Prescription Drug Inflation Rebate Program; specifically Section II K, addressing payment for skin substitutes, 90 Fed. Reg. 32352, 32512-32523.
Venture is a specialty distributor of advanced wound care products including skin substitute products (also referred to as CTPs or CAMPs). Venture has extensive experience in the wound care space and serves the full spectrum of wound specialists including mobile providers, office-based providers, and hospital outpatient providers. Venture has experience with multiple skin substitute product types as well as other wound care technologies including negative pressures, ultrasonics, antimicrobials, and diagnostics.
We know through our own experience, confirmed by extensive recent research and publications, the value of skin substitutes in managing Medicare patients with chronic wounds.
We appreciate and acknowledge the attention that CMS has given to skin substitute reimbursement in the currently proposed PFS. We acknowledge that there have been abuses in this area, driven mostly by the activities of a very small number of providers who have misused the skin substitute product category while not providing adequate standard wound care. We also understand CMS’s inclination to move away from the ASP system towards a different reimbursement structure, which contains cost growth and equalizes reimbursement among products and among sites of care.
However we believe that the currently proposed structure and rate ($125.38/cm2) would restrict or eliminate patient access to critically needed care, especially for rural and underserved patients; restrict innovation and undermine the future progress of skin substitute technology generally; and favor less-expensive, less-effective products, including products from foreign manufacturers. We also suggest that the pending future- effective LCDs are dangerous and unnecessary regulation and should be withdrawn in light of CMS’s reformation of the skin substitute payment methodology.
Venture Supports the Consensus Position of Clinicians, Experts, and Industry
We support the consensus proposal developed by Dr. William Tettelbach and many other clinical, industry and reimbursement experts, and endorsed by multiple clinician groups including the American Professional Wound Care Association (APWCA); the Limb Preservation Foundation (LPF); the Independent Wound Specialist Society (IWSS); the American Board of Wound Healing (ABWH); and the American College of Hyperbaric
Medicine (ACHM). Tettelbach et al., Safeguarding access, fiscal responsibility, and innovation: a comprehensive reimbursement framework for CAMPs to preserve the
Medicare Trust Fund, Journal of Wound Care, https://doi.org/10.12968/jowc.2025.0396. This paper provides a detailed analysis of the issues with the PFS skin substitute proposal and proposes well-thought-out alternatives.
The Methodology Used to Calculate The Reimbursement Rate is Improper
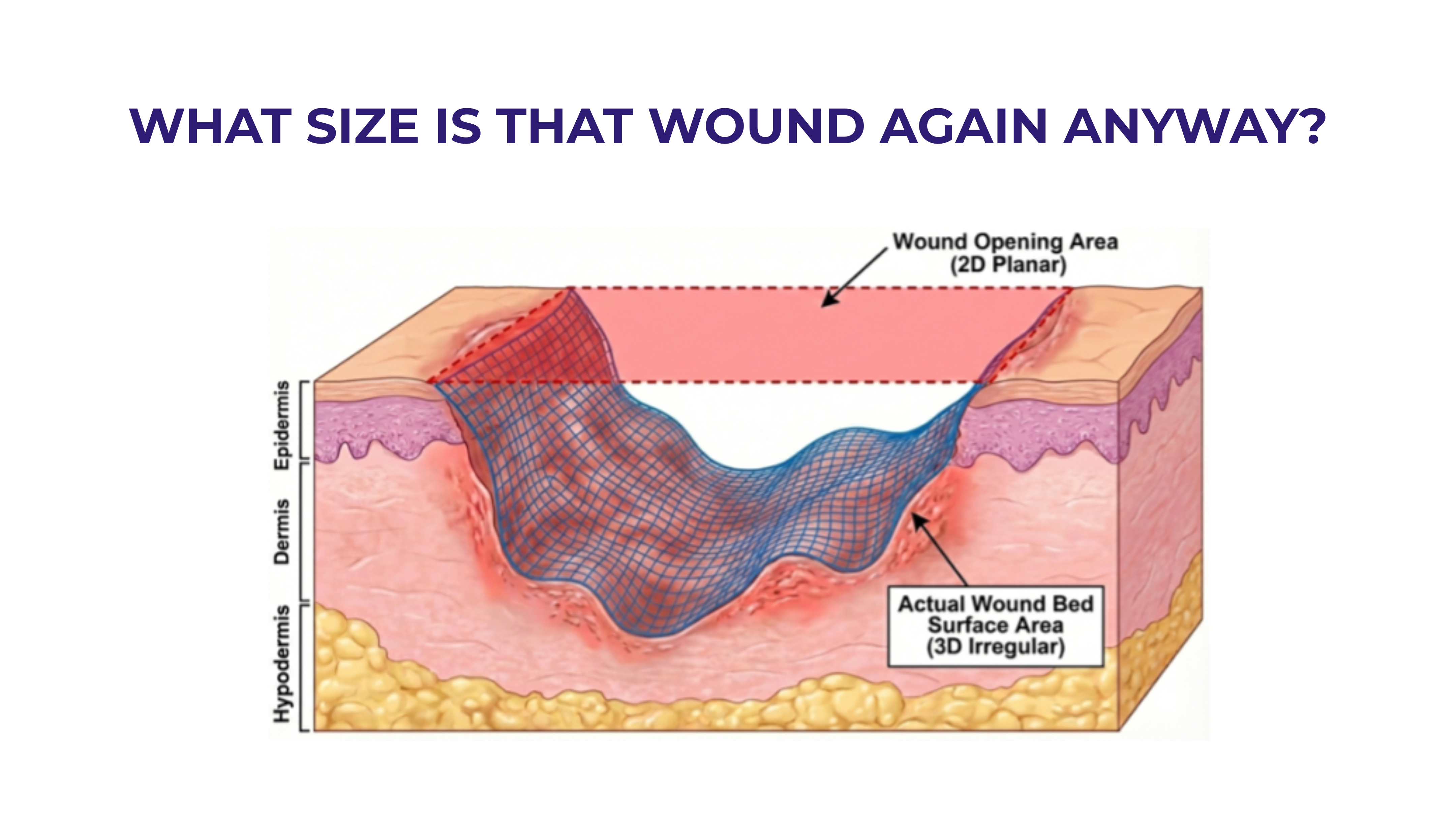
To calculate the proposed rate of approximately $125.38/cm2, the volume-weighted average of ASPs for skin substitutes was used, but the weighting was based only on use in the hospital outpatient site of service. Usage and cost of skin substitutes in physician practices, where the proposed Physician Fee Schedule will actually be applied, was entirely ignored.
The decision to ignore actual practice costs in determining the PFS practice rates is unprecedented and inappropriate. Hospital outpatient departments operate in a very
different economic and clinical environment from physician practices and different products are used. Some products that are popular in the outpatient department are largely unusable in the physician practice environment due to temperature-controlled storage requirements and very short expiration dates. Furthermore, hospitals are part of powerful buying groups which buy in large volumes and have very low credit risk. As a result, hospitals are able to acquire products at significantly lower prices that suppliers can afford to provide to individual practices, which offer lower sales volumes at greater effort and higher risk. Finally, the current bundled reimbursement scheme in the HOPD
tends to distort the market, restricting skin substitute choice and limiting hospital wound clinics to smaller, less severe wounds which may call for less advanced products. The HOPD certainly does not represent an “undistorted” pricing market for skin substitute products and HOPD cost levels are not applicable to the cost structure of physician practices.
We support the idea of setting consistent reimbursement systems for the office and HOPD, as well as removing the artificial limit on the treatment of large wounds in the HOPD.
However, when setting the rate, CMS should undoubtedly take into account weighted product usage in all relevant settings of care. Based on the work of Tettelbach and others, we suggest that a rate in the range of $700 per square centimeter would be appropriate to ensure patient access to care and maintain innovation and correspond to the health economics value of this important class of products.
Given our experience with multiple wound care product manufacturers, we wish to especially highlight the impact of a lower reimbursement rate on the future of technological innovation in skin substitutes and in wound care more generally. The cost of developing a new technology including research, clinical studies commercial launch and scaling is extremely high. Reimbursement in the range CMS currently proposes may (barely) support the cost structure of legacy manufacturers with legacy technologies. It simply will not support the investment required to develop and launch new products. Adoption of the currently proposed rates will drive many products out of the market entirely (a result which would be dramatically accelerated were the proposed future effective LCDs to take effect as written). This rate would also permanently chill new product innovation in skin substitutes, and likely in the broader wound care market as a whole as investors take note of the way in which a sudden CMS change in direction destroyed investor equity across an entire class of products. We urge CMS to prevent this result by adopting a more appropriate and less draconian reimbursement rate.
Application Fees Should Also Be Equalized Between Sites of Care
We also support CMS’s decision to retain a substantial facility fee component for the application of skin substitutes in the HOPD, in addition to separate payment for the product. This ensures fair reimbursement for the clinical work involved as well as the economic risk and stress of purchasing skin substitute products for patients and reduces the pressure to use less-expensive, less-effective products to make the application of skin substitutes more economically feasible for providers.
However, if the PFS and OPPS systems are to be equilibrated, as CMS has indicated is its intent, the clinical fee paid under the physician fee schedule is far too low. Under the current proposal, the HOPD would receive a facility fee of $746.61 plus an additional physician fee of almost $100, while a physician applying a skin substitute in his or her office would receive about $150 total, over 80% less. Some difference in price structure between the hospital clinic and office may be supportable, but this gap is far too large. The skin substitute application fee components of the PFS should be revisited and raised substantially to more closely align reimbursement for skin substitutes in the HOPD and physician practice. Otherwise, CMS would be significantly favoring care in the (more expensive) HOPD and causing an increasing overload of those facilities while undermining the physician offices and mobile practices that care for a majority of Medicare beneficiaries, especially those in rural and underserved area.
Increased Reimbursement Should be Based on Clinical Evidence, Not FDA Status
We appreciate CMS’s suggestion that reimbursement rates after 2026 might be differentiated based on the clinical value of the various products. The one-size-fits-all flat- rate reimbursement framework “disregards clinical nuance and disease severity. Lower- cost therapies are not supported by evidence demonstrating equivalence to more effective biologic or composite CAMPs, such as placenta-derived allografts, which have been shown to significantly reduce mortality, recurrence and adverse outcomes in patients with lower extremity diabetic ulcers (LEDUs) or venous leg ulcers (VLUs)”(Tettelbach et al., early view, 2025).
However, we do not believe FDA product classifications are a helpful basis for differentiation between products. FDA classification is based on the source and type of materials making up the product. A different FDA classification does not represent a finding that one product is more or less efficacious than another. Furthermore, there is no established base of evidence that this is the case. To the extent that such evidence exists, it suggests that human amniotic products classified as HCT/Ps are the most effective products available.
Beyond clinical outcomes, there are significant issues with certain products that affect their cost effectiveness and the current market pricing of those products, and which should not be ignored by CMS. For example, one of the primary PMA products, Apligraf, has logistical challenges driven by its very short shelf life. More importantly, because there is only one large size of this product available, use of this product generates significant waste when applied to most chronic wounds which tend to be significantly smaller. Consider a very common chronic wound size of 4 sq cm. The Apligraf product is only available in a 44 sq cm size. Therefore, application of this product to the wound involves 4 sq cm of useful product, and 40 sq cm or 91% of waste. Even if Apligraf and another product, such as an amniotic product available in a 4 sq cm sheet, were to be reimbursed at the same per sq cm rate, the Apligraf product would cost more than ten times more due to the level of waste. For this reason, Apligraf’s per sq cm reimbursement rate should certainly not be higher than an amniotic product and arguably should be lower.
Rather than basing pricing differentiation on FDA classification, we suggest that comparative clinical evidence is the only appropriate basis of pricing differentiation. We suggest that CMS should equalize reimbursement for all skin substitute products for 2026 as proposed, but continue to work with industry and the clinical community to develop a strategy to provide additional reimbursement to support innovation and clinically proven product effectiveness in future years.
CMS could implement additional payment for innovative skin substitute products, e.g., those that offer markedly improved healing outcomes or reduced complications as demonstrated by clinical data. CMS could do so by implementing codes that would generate additional payment for an initial three-year period if manufacturers can meet certain substantial clinical improvement metrics. The framework could be modeled after the New Technology Add-on Payment (“NTAP”) program in the Inpatient Prospective Payment System (“IPPS”) or the OPPS Pass-Through Status program but should be applicable to the PFS as well as the OPPS. CMS could consider implementing a payment rate of 165% of the decided upon PFS payment rate that would otherwise apply to the product similar to the NTAP payment methodology, or it could adopt a pass-through payment structure. Either would encourage evidence-based innovation by skin substitute manufacturers instead of defaulting to introduction of more “me-too” products into the market.
If CMS proceeds with the proposal to establish categories of payment after 2026 based on the three FDA regulatory pathways, then it is essential that CMS also establish a new category dedicated to advanced allograft products. This category, which we refer to as “HCT/P+,” should recognize those products supported by RCTs and comparative RWE, and which rely on advanced, patented manufacturing processes.
The Future Effective LCDs Should be Rescinded
As the Tettelbach consensus also recognizes, the future effective “national” skin substitute LCDs represent unnecessary and misguided regulation and should be withdrawn. While originally designed to contain reimbursement growth in the absence of CMS pricing reforms, these LCDs are now unnecessary and counterproductive. With reimbursement on a level playing field, clinicians are in a far better position to assess the clinical value of specific products in light of the individual needs of their patients than the MACs.
Regulations that unduly restrict the products available and the treatment decisions of clinicians will only result in less effective care, reduced patient access, and a massive chill on innovation. The LCDs should be withdrawn, and any future LCDs should offer general guidelines for skin substitute usage across all wound types and should not attempt to “pick and choose” products in the place of clinicians.
Sincerely,
John Schroeder
Chief Executive Officer
Venture Medical, LLC







.svg)



.jpeg)