When “Administered” Meets Reality: Why Measuring Wounds for Skin Substitutes Isn’t as Simple as It Seems
CMS’s 2026 wastage proposal reduces billing to “administered” units, but defining what’s truly administered exposes a major gap between policy assumptions and wound-care reality.
The Centers for Medicare & Medicaid Services’ (CMS) proposed 2026 skin substitute wastage policy introduces a deceptively simple rule: providers may bill only for units that are “administered,” not for those that are “discarded.”
On paper, this sounds straightforward. In practice, it opens the door to an extremely complicated measurement problem.
Once wastage is eliminated, a new question takes center stage: What exactly counts as “administered”?
Many assume the answer is simple. Measure the wound, select a graft that matches that measurement, and apply it. Anyone who treats complex wounds knows this is far from reality.
The Core Problem: What Do We Mean by “Wound Area”?
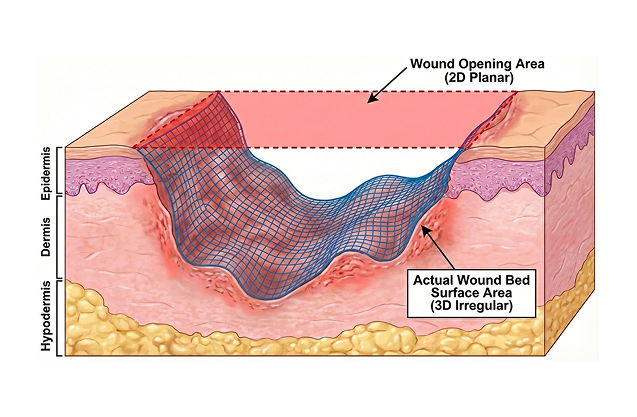
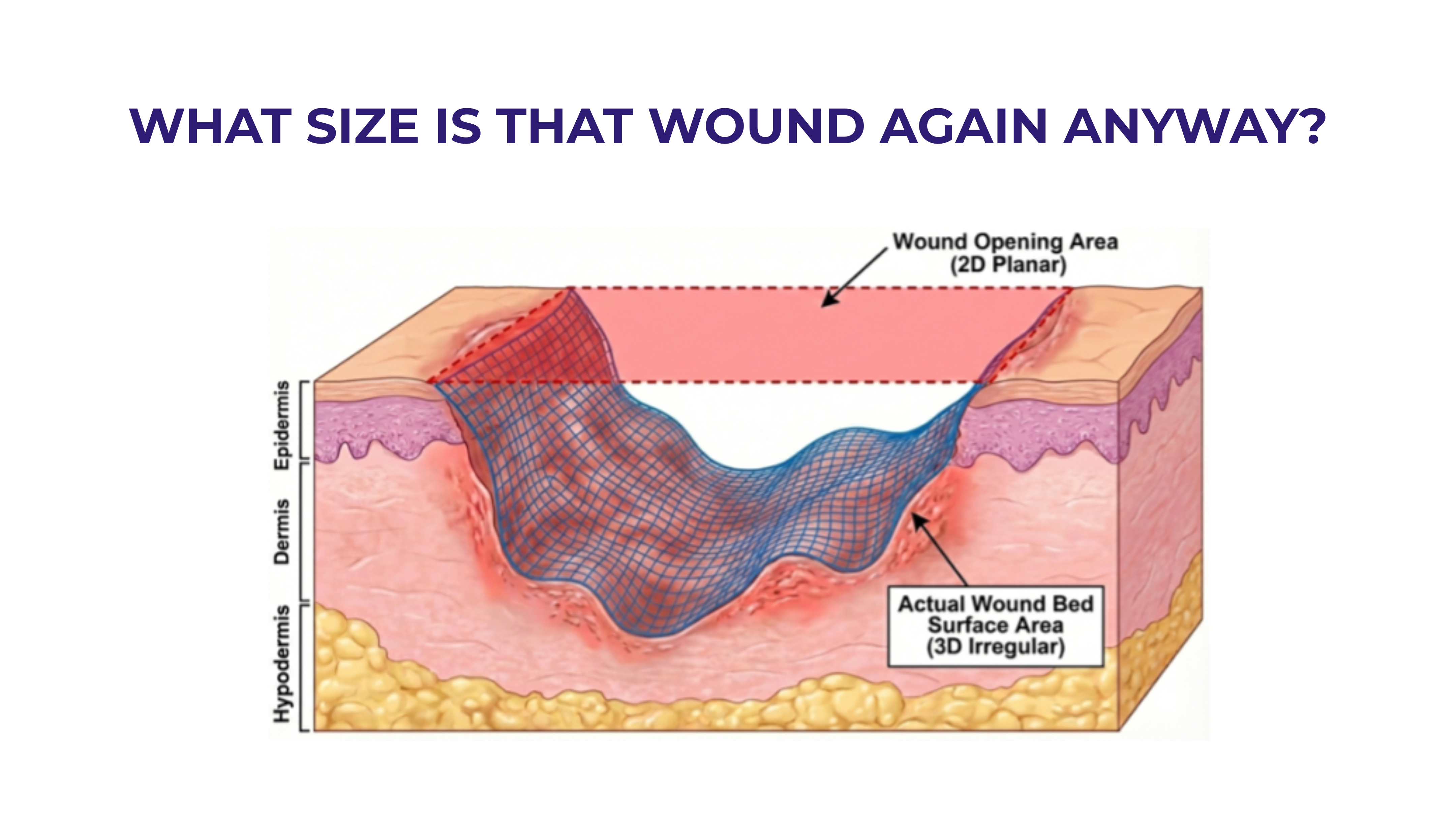
When clinicians talk about wound size, they are often referring to one of two very different measurements: The 2D wound opening area (the area of the opening at skin level) that is historically estimated using length × width or the 3D wound bed surface area (measuring the total internal surface of the wound, including sidewalls, tunnels, and irregular contours). One clinician captured this distinction perfectly, “It’s a little like painting a room. Do you want to just paint the ceiling, or do you want to paint the walls too?”
For skin substitutes to function as intended, and to remain compliant with FDA labeling, they should contact and protect the wound bed itself. That means the 3D wound bed surface area is the clinically relevant measurement.
The Hidden Scale of the Difference
Most people underestimate how large the gap can be between 2D opening area and true 3D wound bed surface area.
Using basic geometric models:
- Shallow wounds: up to ~20% larger than the opening
- Moderate-depth wounds: up to ~100% larger
- Deep or complex wounds: up to 400% larger—or more
And these are conservative estimates.
Importantly, none of this can be accurately calculated with simple L × W × D formulas. Measuring true wound bed surface area requires full 3D surface mapping, which is technologically challenging measurement when it can be done at all.
Estimation Exists; Precision Does Not
Shaun Carpenter, MD, CWSP, DABWMS has proposed a clever drape-based estimation method to better approximate wound bed surface area. Techniques like this move the field forward. But even with innovative approaches, a highy precise, standardized, and widely available method for measuring 3D wound bed surface area does not exist. This means any policy framework that assumes centimeter-by-centimeter precision is operating ahead of real-world capabilities.
Edge Overlap: The Second Multiplier
Depth isn’t the only factor that expands required graft size. Many skin substitutes require overlap beyond the wound margins to:
- Cover wound edges
- Facilitate fixation
- Meet manufacturer Instructions for Use (IFUs)
Even a conservative 0.5 cm overlap around the perimeter can dramatically increase the required graft area:
- Small wounds: additional 100–200% of the wound opening area
- Large wounds: often 25% or more additional area
This overlap is not optional. It is frequently part of proper application technique.
So What Size Skin Substitute Should Actually Be “Administered”?
The most honest answer is, it varies widely.
Appropriate graft size depends on:
- Wound depth
- Geometry and irregularity
- Presence of undermining or tunneling
- Required edge overlap
- Product-specific handling and fixation requirements
In many cases, the clinically appropriate graft is substantially larger than the 2D wound opening measurement.
This is not waste. This is not inefficiency. This is geometry and biology.
The Risk of Oversimplification
A policy environment that implicitly expects: “Measure the wound opening → pick a perfectly matched graft → zero excess”, simply ignores wound care reality.
The Best Measurement Tool We Have Today
Given all the variables that must be considered, the most reliable measurement system we have is clinicians at the bedside. Their assessment should include:
- Visual assessment
- Tactile examination
- Clinical judgment
- Thorough documentation
- Wound photography to support rationale
Digital tools if available can add consistency and strengthen the record. Clear documentation explaining why a specific graft size was selected is currently the strongest bridge between clinical reality and administrative requirements.
There is and should be considerable latitude left to clinicians in fitting specific grafts to the unique needs of specific patients and specific wounds. Clinicians should “administer” the size of graft needed to do the job.







.svg)



.jpeg)